“Doctors maxed out – cost pressure instead of patient welfare”
ZDF report brings up the painful subject of the German health system
by Winfried Pogorzelski
In the series “ZDF-Zoom”, on 28 January 2021, the “Zweites Deutsches Fernsehen” broadcast a film with the title “Ärzte am Limit – Kostendruck statt Patientenwohl. Krankenhausärzte in Deutschland schlagen Alarm (Doctors maxed out – cost pressure instead of patient welfare. Hospital physicians in Germany sound the alarm” on the subject of health care provided to the population of Germany by hospitals. It was about the consequences of the fact that German hospitals have been increasingly transformed into commercial enterprises in recent years, where the primary aim is to operate profitably and avoid financial losses. By now, the patients’ well-being is apparently no longer the top priority, and this scandalous development also comes hard to doctors, nurses and not least the training and further education of specialists. Quite a few of those affected are therefore thinking of giving up their profession or going abroad. However, in this report it remains in the dark how things could come to this.
The physician as a manager: Profit instead of patient welfare
If a profit is to be made from people’s illness, then savings have to be made on materials and staff, to the detriment of the sick, but also to the chagrin of the doctors. There is, for example, the doctor Friederike Schlingloff. She worked in heart surgery at a hospital for eight years and suffered more and more from constant cost and time pressure, which meant that she could not do justice to the patients. Finally, she gave up this kind of work, became an emergency doctor and can now do more for her patients than before in the hospital, namely the best without any ifs and buts.
She also works as a training assistant in a community practice and is for the first time experiencing how beneficial it is to treat a patient according to the motto: “It will take as long as it takes.” Hospitals, on the other hand, usually work at their limit due to chronic staff shortages, resulting in many facilities being unable to admit far too few if any emergency patients. More avoidable serious illnesses and deaths are the result.
The financial pressure results from the introduction of case-based flat rates, the so-called Diagnosis Related Groups, which were introduced in 2003. 12,000 medical services are listed, together with the amount of money they bring. For example, the insertion of a pacemaker brings a gain of 16,000 euros, an operation on the spine 10,000 euros. The amount of the latter procedure increased by a whopping 71 % between 2007 and 2015. Careful discussion of alternative and cheaper treatments before an operation – by rights a matter of course – usually falls flat, because they are not on the list and bring in nothing.
Risks and side effects
On average, only 7.6 minutes are left for a patient consultation; every minute counts. Doctors who do not record their times accurately pay a fine. The principle stemming from the productive economy and used here is called “process control”. 60-hour weeks and 24-hour shifts are not uncommon. A comparison with aviation illustrates what is at stake here: what traveller would board an aircraft whose pilot has, for example, been on duty for thirty hours without interruption?
The future of the health system is also affected, as the training of young doctors suffers under these conditions. According to a survey by the Marburger Bund – the federal association of salaried and civil servant doctors – 70 % of future specialists no longer receive structured further training because there is simply no time for it. As a result, younger specialists are often unable to perform more complex procedures.
Tübingen University and Children’s Hospital – an example
The University Children’s Hospital – Department of Paediatrics in Tübingen treats 12,000 patients a year. As elsewhere, maintenance here costs much more than it yields. In the past, there were no financial discussions because there were no financial constraints, says the health director, but now not a day goes by without debates about money. The so-called commercial director of the clinic repeatedly criticises the hospital for using too much money and earning too little – an accusation that was never heard before. The situation has come to such a heat that the threat of closure is constantly hanging over the hospital like a sword of Damocles. However, the doctors may under no circumstances be forced to practice “unethical medicine”.
The director of the university hospital, Professor Dr Michael Bamberg, reports that the Covid-19 pandemic hit the hospital like a tsunami. Half the necessary operations had to be postponed; 250 patients had to be treated for Covid-19, 36 of them had to be artificially ventilated at the same time. 86 patients with severe cases were treated for four long months. The deficit was in the two- to three-digit million range. Hospitals were stuck with the costs because the subsidies from the state government were a drop in the ocean. One is tempted to say the Covid-19 virus and its mutants also have their good side, they teach us how existentially important a functioning health system is for our society.
Doctors are constantly in conflict, have a guilty conscience because they cannot meet all the demands made on them. In this context, the medical ethicist Professor Dr Giovanni Maio (University of Freiburg i. Br.) speaks of a “moral dissonance”, to which the constant role conflict leads, of conflict situations that should not arise. Burnout and feelings of being drained are the consequences for the individual, the migration of staff and the resulting shortage of doctors and nurses the logical consequence for the health system – a veritable vicious circle, especially since the training of new nurses is expensive, takes many years and the profession is becoming less and less attractive.
How important are public health and the health system truly to us?
There are 1925 clinics in Germany; they have now become veritable health factories and cost around 110 billion euros per year. Their operation is trimmed to efficiency instead of focussed on the patients’ health and well-being. Giovanni Maio speaks of an “economic tribunal” set up against clinics: Everything done there is evaluated according to whether it brings in revenue. The motto is: operate as much as possible, make full use of every minute in the operating theatres. “You can make a lot of money in this way. The doctors don’t even actually want to take a decision in that direction, but they are forced to [...] because they are threatened that their department will be closed,” says Giovanni Maio.
There is no way around a fundamental discussion about how much our health system matters to our society. Professor Peter Rosenberger is the Tübingen University Hospital Medical Director; he is calling for a rethink. The pandemic has made clear the relevance of hospitals, he says. “What I would like to see: a really sustainable change in the world of work, less shaped by monetary factors, less shaped by process controls and financial backgrounds [...]. Perhaps the conclusion to be drawn from the pandemic is that society should discuss the question: How important is the health system to us? Perhaps it is not just about a cost factor, but perhaps it is a very strong pillar of society that no-one has to be afraid of dying from an illness.”
How it could come to this and the increase of resistance
The report only hints at the background of and true reasons for this fatal development of the health system, so here are a few additions: The tendency in our western societies to privatise areas of the public service in order to capitalise on it in the truest sense of the word has a long history. It already began after the German reunification in the times of the government of Helmut Kohl (CDU) and his health minister Horst Seehofer (CSU); under the Red-Green government of Gerhard Schröder (SPD) and Joschka Fischer (The Greens); the DRG (Diagnosis Related Groups) system’s flat rate per case was made compulsory in 2004. If the costs are exceeded because a treatment takes longer due to complications or delays, the additional costs are not covered by the health insurance; hospitals are the sufferers; they are left to bear costs.
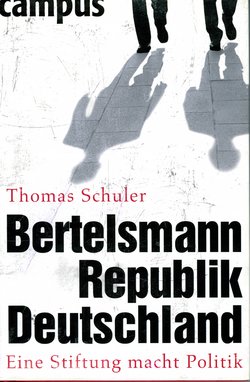
Meanwhile, the hospital business has become a highly lucrative business from which private clinics, nursing homes, the pharmaceutical industry and shareholders profit. The system works according to the principles of competition and profit. Those who cannot hold their own on the free market are out of luck and are cast off. The most important private player in this system is the Bertelsmann Foundation (360 employees, annual budget 60 million euros), behind which stands the Bertelsmann Group, the largest media corporation in Europe, which is very well networked with many private hospital groups such as Rhön-Klinikum AG or Sana-Kliniken. The foundation claims to want to improve the health system. In blatant contradiction to this, it permanently advocates a reduction in the number of hospitals according to the motto “less state, more competition”, arguing that this is the only way the remaining facilities can be run economically. Also, the current government under Chancellor Angela Merkel and Health Minister Jens Spahn are continuing down this fatal path.
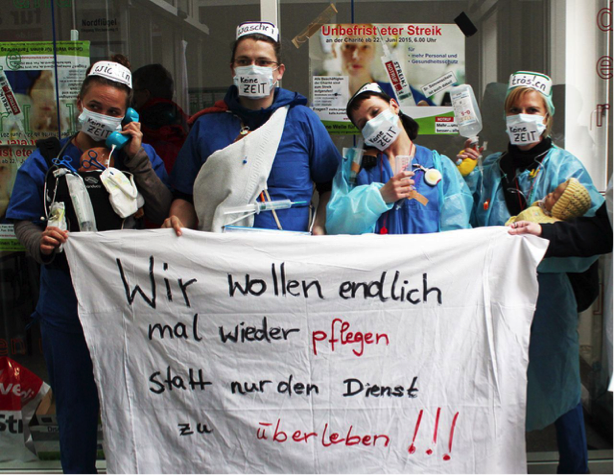
And resistance is rising, first and foremost among those are primarily affected, apart from the patients, namely the doctors. In the Ärzteblatt, the members’ journal of the German medical associations, critical articles on the privatisation of the health system are appearing time and again. Or in the form of an initiative called “Gemeingut in BürgerInnenhand” (Public Property in the Citizens’ Hands), which campaigns for preserving public goods and services and preventing the privatisation of further areas, because otherwise common goods would become commodities, and this would lead to the dismantling of democratic control and local self-government. The work and activities of the Bertelsmann Foundation are repeatedly analysed critically by non-fiction authors.
The hope remains that the current biggest crisis since the Second World War could give the impetus for a turnaround, so that in future the population will once again be able to rely on a well-functioning health system, and people working in the medical and nursing professions will find humane working conditions and regain a joy in their work.
The worrying developments in the health system will bother and preoccupy us for some time to come, and besides, they are also ongoing in Switzerland, as a recent two-part documentary on Swiss television shows. •
Sources:
- “ZDF-Zoom”: “Ärzte am Limit – Kostendruck statt Patientenwohl (Doctors maxed out – cost pressure instead of patient welfare. Hospital physicians in Germany sound the alarm)” by Wieskerstrauch, Liz; Wortmann, Robert, video available until 28 January 2022, https://www.zdf.de/dokumentation/zdfzoom/videos/zdfzoom-aerzte-am-limit-dgs-100.html
- Müller, Albrecht. NachDenkSeiten – The judicial website: https://www.nachdenkseiten.de/?p=5228
- Mertin, Ansgar. “Privatisierung von Kliniken auf Kosten der Patienten.“ (Privatisation of clinics at the expense of patients). In: Der Spiegel, https://www.spiegel.de/gesundheit/diagnose/privatisierung-von-kliniken-auf-kosten-der-patienten-a-909728.html
- Rudolphi, Markus. “Folgen der Privatisierung von Krankenhäusern: Die Spielregeln sind willkürlich. (Consequences of the privatisation of hospitals: The rules of the game are arbitrary.)” In: Deutsches Ärzteblatt 2007; 104 (27): A-1956 / B-1728 / C-1664, https://www.aerzteblatt.de/archiv/56239/Folgen-der-Privatisierung-von-Krankenhaeusern-Die-Spielregeln-sind-willkuerlich
- On 4 and 11 March 2021, Swiss television SRF 1 broadcast a documentary by Michael Zollinger and Pasquale Ferrara, on the current development of the hospital system in Switzerland: “Wettkampf der Spitäler – Weniger Spitäler = bessere Qualität? (Competition between hospitals – Fewer hospitals = better quality?)” (1), “Wettkampf der Spitäler – Mehr Qualität für Patienten oder teures Aufrüsten? (Competition between hospitals – More quality for patients or expensive upgrading)” (2)